
How Many Embryos Are Cultured in the IVF Process?
April 9, 2025
How Many Eggs Are Cultured in the IVF Process?
April 9, 2025What Is the IVF Procedure? Your Complete Guide to In Vitro Fertilization
What Is the IVF Procedure? Your Complete Guide to In Vitro Fertilization
Starting a family can feel like a dream come true, but for some, the path isn’t as simple as they’d hoped. If you’ve been trying to conceive without success, you might have heard about in vitro fertilization, or IVF. It’s a term that pops up a lot these days—on TV, in conversations, or maybe even from a friend who’s been through it. But what exactly is IVF? How does it work, and could it be the key to building the family you’ve always wanted?
IVF is more than just a medical procedure; it’s a journey filled with hope, science, and a little bit of wonder. In this guide, we’re diving deep into what IVF is all about. We’ll walk you through every step, answer your burning questions, and share practical tips to help you feel prepared. Plus, we’ll uncover some lesser-known details—like how recent advancements are changing the game and what real people wish they’d known before starting. Whether you’re just curious or seriously considering it, this is your one-stop resource for understanding the IVF procedure.
The Basics: What Does IVF Actually Mean?
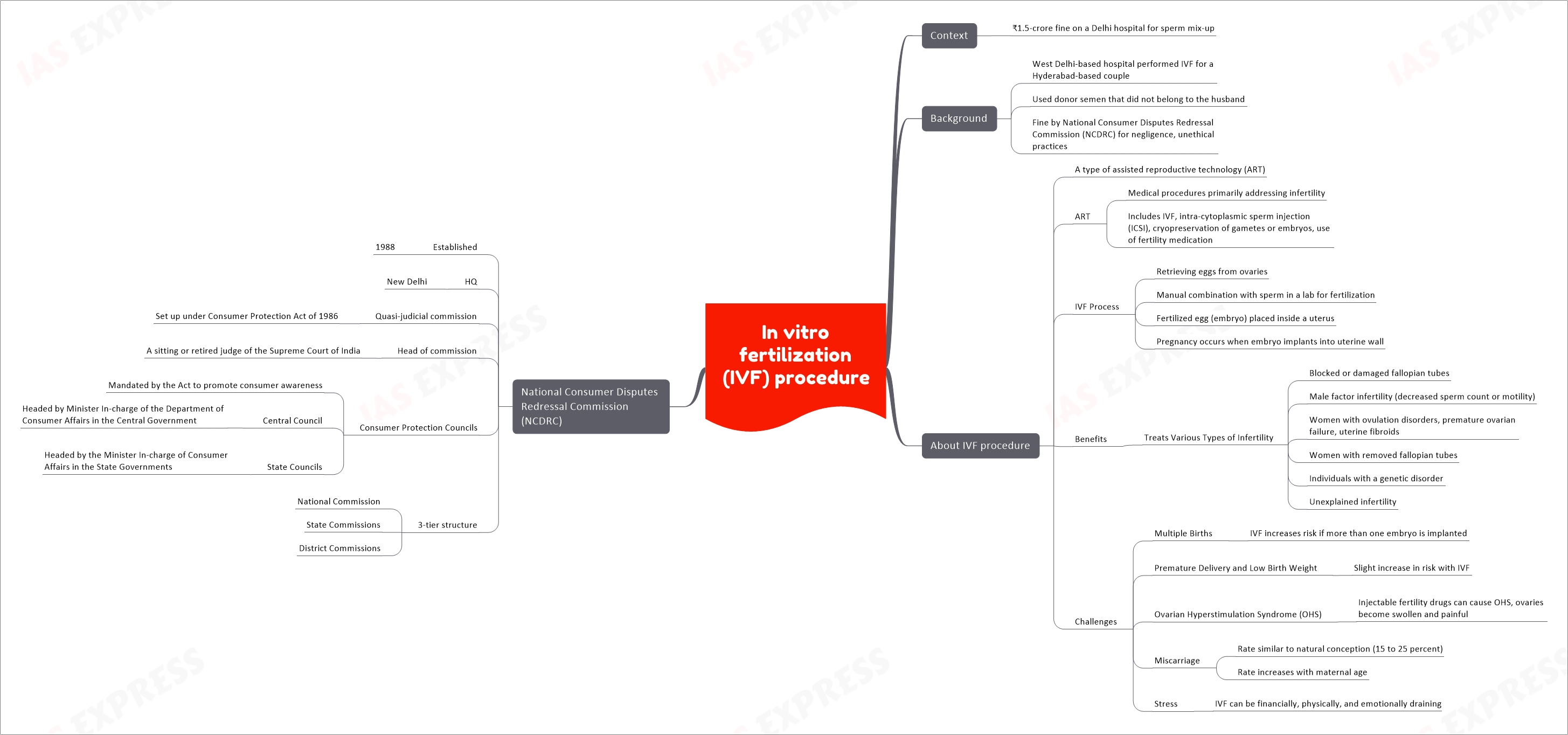
IVF stands for in vitro fertilization. That’s a fancy way of saying fertilization happens outside the body—“in vitro” literally means “in glass,” like in a lab dish. Unlike natural conception, where sperm meets egg inside the fallopian tubes, IVF brings them together in a controlled environment. Then, once an embryo forms, it’s placed into the uterus to grow into a baby.
Think of it like giving nature a helping hand. It’s a process designed for people facing challenges like blocked tubes, low sperm count, or unexplained infertility. Since the first IVF baby, Louise Brown, was born in 1978, millions of families worldwide have welcomed little ones thanks to this technology. Today, it’s one of the most common and successful fertility treatments out there.
But IVF isn’t a one-size-fits-all solution. It’s a multi-step process that takes time, patience, and a bit of courage. Ready to see how it all unfolds? Let’s break it down.
Step-by-Step: How the IVF Procedure Works
IVF isn’t something that happens overnight. It’s a carefully planned series of steps, usually taking 3 to 6 weeks for one full cycle. Here’s what you can expect, explained in a way that’s easy to follow.
Step 1: Boosting Your Egg Supply with Stimulation
The journey starts with your ovaries. Normally, you release one egg each month during ovulation. But in IVF, doctors want more eggs to increase the chances of success. To do this, you’ll take hormone medications—usually injections—for about 10 to 14 days.
These meds tell your ovaries to produce multiple eggs at once. You’ll visit the clinic often during this phase for blood tests and ultrasounds to check how your eggs are growing. It’s a bit like tending a garden: the goal is to nurture as many healthy “seeds” as possible.
- ✔️ Tip: Keep a small notebook to track your appointments and how you’re feeling—some people notice mild bloating or mood swings from the hormones.
- ❌ Don’t: Skip doses or appointments; timing is everything here.
Step 2: Collecting the Eggs
Once your eggs are ready—usually when they’re about 18-20 millimeters in size—it’s time for retrieval. This happens around day 12 to 14 of your cycle. You’ll get a light sedative (no heavy anesthesia needed), and a doctor uses a thin needle guided by ultrasound to gently collect the eggs from your ovaries.
It sounds intense, but it’s quick—about 20 minutes—and you’ll rest for a bit afterward. Most people describe it as mildly uncomfortable, like period cramps, rather than painful.
- Fun Fact: The average number of eggs retrieved is 8 to 15, though it varies based on age and health.
Step 3: Bringing Sperm and Egg Together
Now comes the magic moment: fertilization. If you’re using a partner’s sperm, they’ll provide a sample the same day as egg retrieval. If you’re using donor sperm, it’s thawed and ready to go. In the lab, an embryologist combines the eggs and sperm in a dish.
There are two ways this can happen:
- Standard IVF: Sperm and eggs are mixed together and left to fertilize naturally.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into an egg—super helpful if sperm count or movement is low.
After a day or two, the team checks to see how many embryos (fertilized eggs) have formed. Not every egg will become an embryo, but that’s normal.
Step 4: Growing Healthy Embryos
The embryos spend 2 to 6 days growing in a special incubator that mimics the womb’s conditions. During this time, embryologists watch them closely, looking for strong, healthy ones. By day 5 or 6, the best embryos reach the blastocyst stage—think of it as the “ready-to-plant” phase.
Some clinics use fancy tech, like time-lapse imaging, to monitor growth without disturbing the embryos. This step is crucial because it decides which embryo has the best shot at becoming a baby.
- ✔️ Tip: Ask your clinic if they offer genetic testing (like PGT) to screen embryos for health issues—it’s optional but can add peace of mind.
Step 5: Transferring the Embryo to the Uterus
Here’s where hope turns into action. The doctor picks the healthiest embryo (or sometimes two) and uses a thin catheter to place it into your uterus. It’s a simple procedure—no sedation needed—and feels like a Pap smear. You’ll lie down for a short rest afterward, but then you’re free to go home.
This usually happens 3 to 5 days after egg retrieval. If you have extra healthy embryos, they can be frozen for later use—more on that soon!
Step 6: The Two-Week Wait and Pregnancy Test
Now, you wait. About 10 to 14 days after the transfer, you’ll take a blood test to see if you’re pregnant. This “two-week wait” can feel endless, filled with excitement and nerves. The embryo needs to implant in your uterine lining for the pregnancy to take hold.
- ✔️ Tip: Stay busy with light activities like reading or walking—stress won’t ruin your chances, but relaxing helps pass the time.
- ❌ Don’t: Take a home pregnancy test too early; it might give a false result.
If the test is positive, congratulations—you’re on your way! If not, don’t lose hope; many people need more than one cycle to succeed.
Who Can IVF Help? Common Reasons People Choose It
IVF isn’t just for one type of person—it’s a lifeline for all kinds of families. Here are some situations where it shines:
- Blocked Fallopian Tubes: If your tubes are damaged or blocked, eggs can’t meet sperm naturally. IVF skips that step entirely.
- Male Infertility: Low sperm count or poor motility? IVF, especially with ICSI, can make it work.
- Unexplained Infertility: When doctors can’t pinpoint the issue after testing, IVF often steps in as the next move.
- Age-Related Challenges: As women get older, egg quality drops. IVF can use donor eggs or your own frozen eggs from earlier years.
- Same-Sex Couples or Single Parents: With donor sperm, eggs, or surrogates, IVF opens doors to parenthood.
Real story: Sarah, a 38-year-old teacher, had endometriosis—a condition where uterine tissue grows outside the womb—making natural conception tough. After two years of trying, she and her husband turned to IVF. Their first cycle brought their son, Liam. “It wasn’t easy,” she says, “but holding him made every shot worth it.”
What’s New in IVF? Recent Trends and Breakthroughs
IVF isn’t stuck in the past—it’s evolving fast. Here’s what’s making waves in 2025, based on the latest research and chatter on platforms like X:
Less Medication, More Comfort
Some clinics now offer “mild IVF” or “natural cycle IVF,” using fewer drugs or none at all. It’s gentler on your body and wallet, though success rates can be lower. A 2023 study in Reproductive BioMedicine Online found mild IVF works best for younger women with good ovarian reserves—something to ask your doctor about.
AI-Powered Embryo Selection
Artificial intelligence is changing how embryologists pick embryos. AI analyzes growth patterns and predicts which ones are most likely to implant. A 2024 trial from Fertility and Sterility showed AI boosted success rates by 15% compared to traditional methods. It’s like having a super-smart assistant in the lab!
Freezing Eggs for the Future
More people are freezing eggs in their 20s or 30s to use later. It’s a game-changer for delaying parenthood without losing egg quality. Data from the CDC in 2023 showed a 20% rise in egg-freezing cycles since 2020—proof it’s catching on.
- Interactive Poll: Have you thought about freezing your eggs or embryos?
- A) Yes, I’m planning it!
- B) Maybe someday.
- C) Not for me.
The Emotional Side: What People Don’t Talk About Enough
IVF is a physical process, but it’s also an emotional rollercoaster. Most articles focus on the science, but let’s shine a light on the feelings that come with it—something Google’s top results often skim over.
The Highs and Lows
One day, you’re thrilled about a good ultrasound; the next, you’re crushed if an embryo doesn’t take. It’s normal to feel this tug-of-war. A 2022 study in Human Reproduction found 60% of IVF patients experience anxiety during the two-week wait—yet few clinics offer mental health support.
- ✔️ Tip: Find a support group (online or in-person) to share your story—it’s less lonely when you’re not alone.
Partner Dynamics
IVF can test relationships. One partner might feel guilt if infertility is “their issue,” while the other juggles hope and frustration. Couples who talk openly—like scheduling a weekly “feelings check-in”—tend to navigate it better.
The Hidden Stress of Success
Even a positive test brings mixed emotions. Will the pregnancy stick? What if something goes wrong? Sarah, from our earlier story, admitted, “I was scared to celebrate until the first ultrasound. It’s like you’re holding your breath.”
Costs and Coverage: What to Expect Financially
IVF isn’t cheap, and this is where many hit a roadblock. In the U.S., one cycle averages $12,000 to $25,000, depending on meds, testing, and location. But don’t let that scare you—there are ways to make it manageable.
Breaking Down the Price Tag
- Medications: $3,000–$5,000
- Egg Retrieval and Lab Work: $6,000–$10,000
- Embryo Transfer: $3,000–$5,000
- Extras (like genetic testing): $1,000–$3,000
Insurance and Support
Some states, like New York, mandate insurance coverage for IVF—up to three cycles in many cases. Check your policy or ask HR. If you’re uninsured, look into:
- Grants: Organizations like Baby Quest offer financial help.
- Clinics with Payment Plans: Many spread costs over months.
- Quick Quiz: What’s your biggest IVF cost concern?
- A) The meds
- B) The procedures
- C) All of it!
Success Rates: What Are Your Chances?
Success isn’t guaranteed, but it’s higher than you might think. The CDC tracks IVF outcomes, and here’s the latest scoop for 2023:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50–55% |
| 35–37 | 40–45% |
| 38–40 | 25–30% |
| Over 40 | 10–15% |
- Key Insight: Using donor eggs bumps success to 50–60%, even for older women.
Lifestyle matters too. A 2024 study in The Lancet found that cutting caffeine (under 200 mg/day) and maintaining a BMI of 19–25 improved outcomes by 10%. Small changes, big impact.
Risks and Side Effects: What to Watch For
IVF is safe, but it’s not risk-free. Here’s what you should know:
Common Side Effects
- Bloating or Cramping: From hormone shots or retrieval.
- Mood Swings: Hormones can mess with your emotions.
- ** Bruising:** At injection sites—ice helps!
Rare but Serious Risks
- OHSS (Ovarian Hyperstimulation Syndrome): Too many eggs can swell your ovaries. It affects 1–5% of cycles and usually resolves with rest.
- Multiple Births: Twins or triplets happen in 15–20% of transfers with two embryos—cute, but riskier.
- ✔️ Tip: Call your doctor if you feel severe pain or shortness of breath—better safe than sorry.
Frozen Embryos: A Game Plan for Later
Got extra embryos? Freezing them is like hitting pause on your family plans. They’re stored in liquid nitrogen at -196°C, and 90% survive thawing, per a 2023 Fertility and Sterility report. You can use them years later—perfect if you want more kids or the first cycle doesn’t work.
Real story: Mike and Jen froze three embryos in 2021. After their daughter was born, they used one in 2024 for a second child. “It felt like a backup plan that paid off,” Mike says.
Unique IVF Options You Haven’t Heard About
Google’s top articles stick to the basics, but IVF has some cool twists worth exploring:
In Vitro Maturation (IVM)
Instead of pumping you with hormones, doctors retrieve immature eggs and mature them in the lab. It’s less invasive and cheaper—around $8,000 per cycle. A 2024 study in Cureus showed IVM success rates hit 35% for women under 35. It’s not mainstream yet, but it’s growing.
Sperm Sorting with Microfluidics
New tech uses tiny channels to pick the fastest, healthiest sperm. It’s like a sperm Olympics—only the champs make it to the egg. Early trials suggest a 20% boost in fertilization rates.
Uterine Microbiome Testing
Your womb’s bacteria might affect implantation. A 2023 pilot study found women with balanced microbiomes had 25% higher success rates. Some clinics now test and tweak it with probiotics—wild, right?
Preparing for IVF: Your Action Plan
Feeling ready to dive in? Here’s how to set yourself up for success:
- Find the Right Clinic: Look for high success rates and good reviews. Ask about their embryo grading system.
- Boost Your Health: Eat a Mediterranean diet (fish, veggies, nuts), sleep 7–8 hours, and skip smoking.
- Talk Money: Get a clear cost breakdown upfront and explore financing.
- Build a Support Squad: Tell a friend or family member—they can cheer you on.
- Checklist: What’s your next step?
- ✔️ Research clinics
- ✔️ Schedule a consult
- ✔️ Start healthy habits
The Bigger Picture: IVF’s Impact on Families
IVF isn’t just about science—it’s about dreams coming true. Over 8 million babies have been born this way since 1978, and that number’s climbing. It’s reshaping how we think about parenthood, giving hope where there once was none.
Takeaways from real families:
- “It’s hard, but it’s worth it,” says Jen.
- “I wish I’d started sooner,” admits Sarah.

